Cutting-Edge Imaging Technologies Advance Care for BPD Center

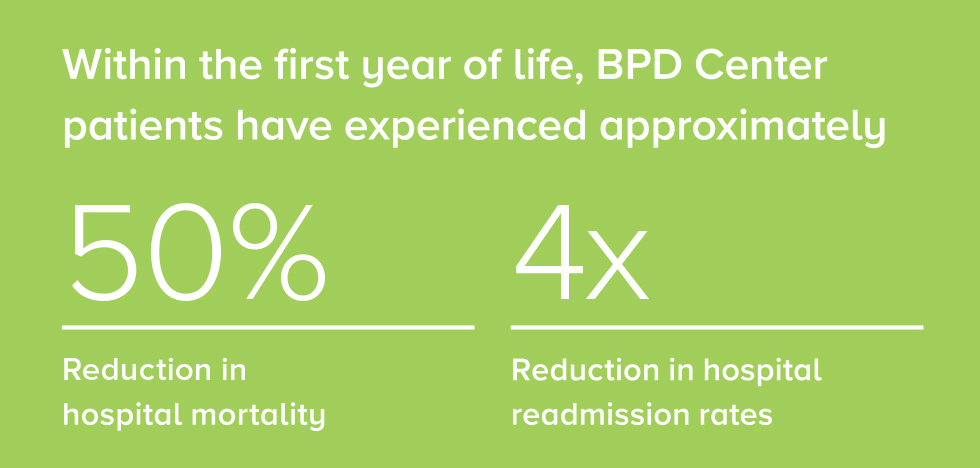
Built on a long history of leadership and groundbreaking research, the Bronchopulmonary Dysplasia (BPD) Center at Cincinnati Children’s was officially established in December 2017. The Center has seen significant improvements in patient outcomes in the two years since its inception. Among infants with BPD, a 50 percent reduction in hospital mortality and a fourfold reduction in hospital readmission rates within the first year of life has occurred among Center patients.
Three co-directors lead this center—pulmonary medicine specialist Erik Hysinger, MD, MS, neonatologist Paul Kingma, MD, PhD, and pulmonary imaging specialist Jason Woods, PhD—combining their expertise for the benefit of preterm babies with lung disease, airway obstruction and pulmonary hypertension. That multidisciplinary collaboration is a hallmark of this center’s approach to care. They work together and bring in specialists from other disciplines, allowing for a more rapid and personalized care approach for the patient.
“The combination of a multidisciplinary team and our advanced imaging allows us to be very precise about the delivery of medical care,” says Woods, who is also director of the Center for Pulmonary Imaging Research. “We believe that will improve both short- and long-term outcomes for these babies.”
Novel MRI Techniques
The imaging Woods refers to includes unique neonatal cardiorespiratory MRI exams, which are performed without sedation and without radiation or increased risk. Their MRI magnet was custom-built, reduced down to the size of a premature infant, and is located right inside of the medical center’s Newborn Intensive Care Unit (NICU). The result is stronger gradients, faster imaging and higher resolution. The team uses this imaging data to guide patient therapy and predict outcomes. “These MRI techniques aren’t available anywhere else in the world,” Kingma says. “They are proving to be better at identifying lung, airway and heart problems than any other currently available methods.”
The opening of this center has also resulted in increased continuity of care for the families of these babies. Coordination of care has improved between neonatology and other departments where these babies often transition to post-NICU, as well as with discharge from the hospital and follow-up visits. And because infants with BPD may continue to have related medical needs as they grow, this team is committed to caring for children from infancy through adolescence.
Research Aids Patients of Today and Tomorrow
Research plays an important role in this team as well. Participating in the latest research and clinical trials allows them to develop state-of-the-art therapies to help the next generation of patients. “There is a great synergy between the clinical and research sides of the team,” says Hysinger. “We have an extremely qualified clinical team that is capable of influencing the research development. And because of that research, we’re able to create tools that are helpful for the clinical team.”
A notable research project currently underway, led by Jeffrey Whitsett, MD, co-director of the Perinatal Institute, is integrating research with the lung map to understand the molecular mechanisms that underlie both normal and abnormal lung development.
This team is energized by the results they’ve seen since the center first opened. With their team approach to care and commitment to making advances in their field, there is no question that they are improving the lives of the children in their care.