Virtual Heart Transplantation Matches More Organs to Recipients in Need
For heart transplantation, achieving a close size match between a donor organ and the space within a recipient’s chest cavity is crucial to success, yet can be especially challenging to achieve when working with children.
This issue, along with many other challenges, has meant that children with end-stage heart failure face the highest waiting list mortality in all of transplant medicine. Now, size-matching complexities have become easier to solve thanks to a 3-dimensional virtual reality process developed at Cincinnati Children’s.
Currently, there are no uniform standards for organ sizing. Transplant groups generally use body weight or height to guide donor selection, but these measures do not consistently reflect chest cavity size.
Exploring Size Matching
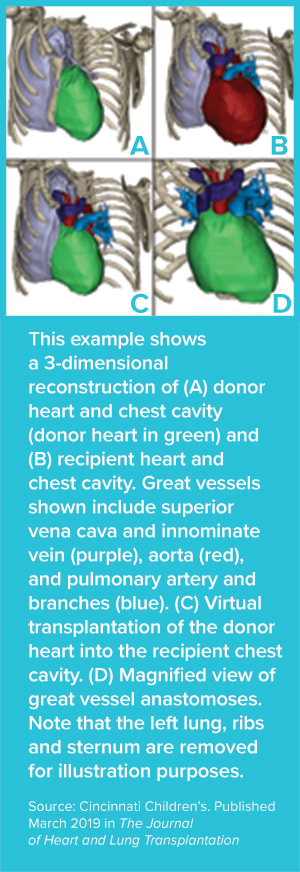
A new study published in March 2019 by The Journal of Heart and Lung Transplantation examined this topic. First author Nicholas Szugye, MD, a clinical fellow in the Heart Institute, and senior author Ryan A. Moore, MD, director of the Heart Institute Digital Media and 3D Modeling Program, led the study. Their research compared four transplant patients with dilated cardiomyopathy (DCM) against a virtual pool of 25 potential donors.
The team found that virtual sizing enabled more donor organs to be acceptable for transplantation. On average, virtual transplantation yielded a maximum donor-recipient ratio of 2.15 or 215% of recipient weight, much higher than thresholds set at most institutions.
Increase in Acceptable Donors
Calculating 3D total cardiac volume (3D-TCV) requires importing chest CT imaging data into a 3D visualization software program and modeling pertinent anatomic structures in order to perform a virtual heart transplant. A candidate organ was considered a fit if it did not interfere with the anterior chest wall or impinge on the descending aorta, left main stem bronchus, left pulmonary veins or lung parenchyma.
“If virtual transplantation is used, the number of acceptable donors for each patient will increase proportionally with the size of the heart rather than the weight of the child,” the co-authors state.
This work will be further explored, along with the many other challenges that transplant patients face, through a recently funded National Institutes of Health Research Project Grant (R01) awarded to co-authors Farhan Zafar, MD, and David Morales, MD, director of Congenital Heart Surgery at the Heart Institute. This work is aimed at improving organ allocation in the heart and lung transplant population.
Additional co-authors included Angela Lorts, MD, and Michael Taylor, MD.

