New Test, Scientific Discoveries Accelerate Diagnosis of Biliary Atresia
A groundbreaking test developed at Cincinnati Children’s can expedite a diagnosis of biliary atresia (BA), helping physicians decide quickly whether to perform a liver biopsy followed by an operative cholangiogram, the definitive test for BA. The test quantifies the concentration of MMP-7 (matrix metalloproteinase-7), a serum protein that researchers at Cincinnati Children’s discovered in 2017 is a biomarker of BA.
Benefits of the MMP-7 Assay
BA is the most common diagnosis leading to liver transplants in children. Early diagnosis and prompt surgical intervention are the best predictors of treatment success, but current diagnostic methods are time consuming, costly and imprecise. Physicians can order the MMP-7 assay by submitting a requisition form. Results are available within 48 hours, and a pediatric hepatologist is available for consultation regarding the interpretation of test results.
“The MMP-7 assay allows physicians to move quickly from an initial impression of BA to the MMP-7 assay, which facilitates a timely decision to conduct confirmatory tests and then the Kasai procedure,” says Jorge Bezerra, MD, director of the Division of Gastroenterology, Hepatology and Nutrition at Cincinnati Children’s.
Introducing this assay for BA is the culmination of several years of research at Cincinnati Children’s. Researchers here published their discovery that MMP-7 is a biomarker of BA in November 2017. Last August, they published a follow-up study in a Rapid Communication (Hepatology, Aug. 28, 2018). The study confirmed that the serum MMP-7 assay has high sensitivity and specificity to differentiate BA from other neonatal cholestasis, and may be a reliable biomarker for BA.
Further Research
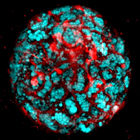
More recently, scientists at Cincinnati Children’s published a study online in the journal Gastroenterology (June 19, 2019) that highlighted two significant discoveries about BA. Bezerra and his colleagues identified an expression pattern of 14 genes at the time of diagnosis that predicts two-year, transplant-free survival in children with the disease. The relationship between a 14-gene signature at diagnosis and two-year survival provides insight into staging of liver disease and the development of new therapies, Bezerra says.
The researchers also found that the antioxidant N-acetyl-cysteine (NAC) reduced liver injury and fibrosis in mice with BA and increased survival times. “A particularly appealing possibility is the development of a clinical trial designed to activate the glutathione pathway—a molecule highly expressed in infants with biliary atresia,” Bezerra explains. “The activation of the pathway by the antioxidant NAC has the potential to improve bile flow and block fibrosis development.”