End-stage Lung Failure Program Provides Hope For Patients With No Other Options

Patients with end-stage lung failure now have a new hope. Physicians at Cincinnati Children’s have created the first program to focus on a comprehensive strategy for end-stage lung failure in children, teens and young adults who seemingly have no other options.
The End-stage Lung Failure Program is for patients with end-stage acute lung failure, chronic lung failure or combined heart-lung failure. It is a collaboration among the hospital’s Heart Institute and Pulmonary and Critical Care divisions.
“Those who may benefit from this program include children who are declining despite all therapies available to them or are at a level of illness from which they cannot move forward,” explains David L.S. Morales, MD, surgical director, Thoracic Transplantation and Mechanical Circulatory Support.
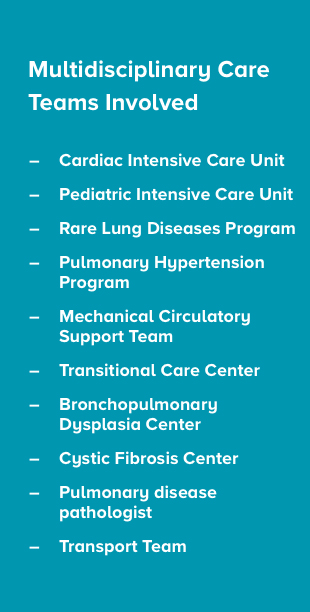
Morales leads the program with Don Hayes, Jr., MD, MS, MEd, medical director, Lung Transplant Program, and David Cooper, MD, MPH, medical director for the Cardiac Intensive Care Unit (CICU) and the Heart Institute.
“The collaboration among multiple teams is a vital component of this innovative approach to care,” Cooper says. “Once the patient is here, we can pull in all the specialists needed to determine whether the patient can either recover from lung failure, or if they need to be bridged to lung transplantation.”
The team has unique expertise caring for patients who are critically ill and require cardio-respiratory support, including advanced techniques of mechanical ventilation, extracorporeal life support—such as extracorporeal membrane oxygenation (ECMO) or paracorporeal lung assist device—or specialized surgeries such as a Potts shunt.
House fire victim receives life-saving care
In 2020, 11-year-old Quintavious was in an Alabama house fire and experienced lung injury due to smoke inhalation. His respiratory support escalated to ECMO with no signs of improvement. His local hospital’s care team called Cincinnati Children’s to discuss the possibility of a lung transplant.
When Quintavious arrived in Cincinnati, the End-stage Lung Failure team identified his needs and directed his treatment plan to recovery rather than transplant. He started to improve despite all odds. He was decannulated from ECMO and removed from the ventilator, then returned to Alabama for inpatient recovery and rehabilitation.
That return to the original point of care is one of the mainstays of this program. “Our goal is to partner with the institution where the patient is to help augment care there, or to transfer to us if necessary and return the patient to them,” Hayes says.
The team is open to consults for any pediatric or young adult patient with end-stage lung failure.

