Neurosurgeons Combine Hybrid OR and sEEG for Safer, More Precise Identification of Seizure Origins

For children with difficult-to-treat seizures, pinpointing seizure origin and location in the brain is a crucial step. For several years, neurosurgeons have used Stereo-electroencephalography (sEEG) for this purpose. Now, neurosurgeons at Cincinnati Children’s have the additional advantage of using the hospital’s Hybrid OR, where they can employ sEEG with robotic assistance, intraoperative imaging and electrocorticography, making the process of implanting electrodes to identify the source of seizures even more accurate and safe for young patients.
“The Hybrid OR allows us to use the robot and minimally invasive technology to do everything in one place,” says Francesco Mangano, DO, director of the Division of Neurosurgery, who has been using the new operating room since May 2020. “Our imaging is immediate. We can see if electrodes are where we want them to be or if there’s a complication. We can manage operative protocols in a much more efficient way.”
Images Allow Precise Placement
The “robot” is a robotic platform that fuses CT and MRI images of the patient’s brain. The fused image provides a highly detailed picture that the neurosurgeons use to determine where to place the electrodes that will monitor seizure activity.
“We load that plan into the robot, and once registration is complete, we drive the robotic arm to entry points on the scalp. It is minimally invasive, but has to be very exact to avoid blood vessels - we are placing these electrodes as deep in the brain as necessary,” says Mangano.
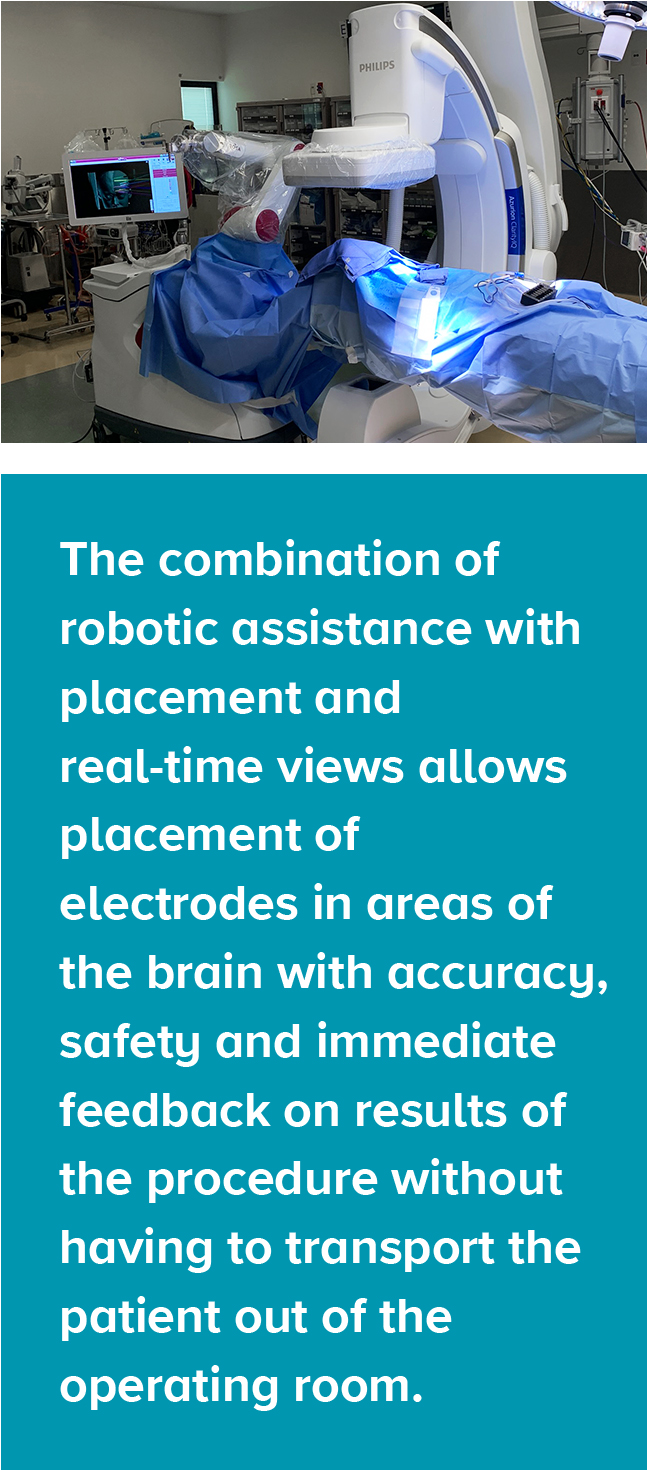
Once the electrodes are placed, the surgeons can view them on a monitor, to make sure they are where they want them to be, or if adjustments need to be made. The combination of robotic assistance with placement and real-time views enable the surgeons to place electrodes in areas of the brain that were previously unreachable, which will provide more accurate identification of where seizures are originating. After surgery, patients are monitored in a special unit from days to weeks to identify where the seizures originate and to identify next steps in care.
Ensuring Greater Safety for Patients
Mangano anticipates performing around 40 such procedures per year, a conservative estimate. Before the Hybrid OR, he says, patients undergoing this procedure would have been moved from one location in the hospital to another while under anesthesia. Now, everything, including intra-op imaging, can be done in one room, and those images can be sent immediately to the hospital’s pediatric neuroradiologists for real-time interpretation expertise.

“This is the safest way we can perform this procedure,” Mangano says. “We can load the plan, perform the plan and evaluate it while the patient is under general anesthesia. If we need to alter the plan based on the imaging, we can do it in real time. The Hybrid OR gives us a better sense of confidence that we will offer patients the least possible opportunity for complications.”

